Peritoneal Mesothelioma
Peritoneal mesothelioma is cancer in the peritoneum, the lining of the abdomen. It is the second most common type of mesothelioma cancer. The most effective form of treatment is a procedure called CRS-HIPEC, which is cytoreductive surgery and hyperthermic intraperitoneal chemotherapy.
Home » National Mesothelioma Law Firm » Mesothelioma Cancer » Types of Mesothelioma » Peritoneal Meso
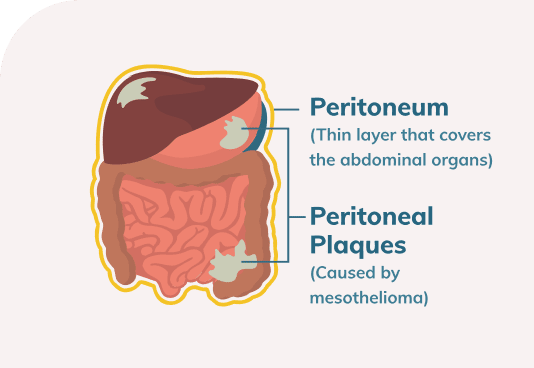
Malignant peritoneal mesothelioma is a cancer that affects the peritoneum, which is the lining of the abdomen. It’s the second most common type of mesothelioma, accounting for approximately 10 to 15 percent of all mesothelioma cases. Although life expectancy without treatment is only a few months, treatment with a particular combination of surgery and chemotherapy known as CRS-HIPEC can increase this by a few years in some patients.
Peritoneal Mesothelioma Risk Factors
Malignant peritoneal mesothelioma is a rare cancer, with about 400 cases per year diagnosed in the United States. It’s found in approximately equal numbers of men and women.
Asbestos exposure is a significant risk factor for the development of this disease. Asbestos is a mineral that was widely used for many years in certain industries due to its extreme stability and high resistance to heat. Workers in some industries were exposed to asbestos on the job; the fibers could also be transported home to their families on their clothing, hair and skin.
Inhaled asbestos can lead to the development of pleural mesothelioma, a cancer of the pleura (the lining of the lungs). Asbestos can also be coughed up and swallowed. It’s such a stable mineral that even stomach acid won’t destroy it, so the tiny fibers of asbestos enter the stomach and intestines.
From there, they can work their way into the peritoneum, the membrane that lines the outside of the digestive tract. Like any foreign substance, asbestos provokes an inflammatory response by the body. This inflammation can alter the DNA of cells, ultimately leading to the development of cancer.
Studies of epidemiology indicate that the link between asbestos exposure and peritoneal mesothelioma is not quite as strong as for pleural mesothelioma. Still, asbestos is clearly linked to peritoneal mesothelioma, and approximately one-third to one-half of all peritoneal mesothelioma patients have a known history of asbestos exposure.
Peritoneal Mesothelioma Symptoms
The symptoms of peritoneal mesothelioma may include:

Nausea and/or vomiting

Diarrhea

Constipation

Loss of appetite

Abdominal pain

Swelling of the abdomen
Unexplained weight loss
These are also common symptoms in a variety of other digestive conditions, including Crohn’s disease, irritable bowel syndrome and colon cancer. Because the symptoms are so nonspecific, the diagnosis of this cancer can be difficult. The average time between onset of symptoms and diagnosis is four to six months.
Peritoneal Mesothelioma Diagnosis
In order to definitively establish the diagnosis of malignant peritoneal mesothelioma, a biopsy is needed. This is a small sample of tissue taken from the tumor. A pathologist will examine the tissue under a microscope and test it in various ways to determine whether there are cancer cells present and, if so, what type of cancer cells they are.
As part of the diagnostic process, it’s important to determine the stage, or how advanced the cancer is. There’s no formal system for determining the stage of peritoneal mesothelioma, but one common method is called the modified TNM staging system. This uses a measurement called the peritoneal cancer index, or PCI. The abdomen is divided into 13 regions, and the amount of cancer present in each region is scored from 0 to 3, for a total PCI of up to 39.
- If the tumor is located relatively close to the skin, a core needle biopsy may be used. A needle is passed through the skin directly into the tumor, often with ultrasound guidance.
- If the patient has a fluid buildup in the abdomen (known as ascites), then this fluid may be drained in a procedure known as paracentesis. In some cases, there are enough cancer cells present in this fluid for the pathologist to analyze. This is sometimes known as a fluid biopsy.
- In many cases, the biopsy is obtained during a minor surgical procedure known as a laparoscopy. Tiny incisions are made in the abdominal wall, and the abdomen is inflated with gas. The surgeon inserts a scope, which allows viewing of the inside of the abdominal cavity using a video camera. In addition, specially-designed surgical instruments can be inserted through the scope to obtain one or more biopsy samples.
- In some cases, the surgeon can’t visualize the tumor well enough using the laparoscope, and a laparotomy may be used instead. This is an exploratory surgery using a longer incision, which allows the surgeon to view the inside of the abdominal cavity directly and obtain biopsies.
Treatment of Peritoneal Mesothelioma
- Cytoreductive surgery (CRS), sometimes known as debulking. The surgeon removes as much tumor tissue as possible from the abdominal cavity. This generally involves removing the omentum, which is a part of the peritoneum that folds down over the front of the abdominal cavity. In addition, other organs (or parts of organs) are often removed, such as the gallbladder, spleen and/or parts of the intestine.
- Hyperthermic intraperitoneal chemotherapy (HIPEC). After removal of tumor tissue, heated chemotherapy medication (most commonly cisplatin) is infused into the abdominal cavity. It's left there for a period of time, and then washed out. This concentrates the chemotherapy at the sites where the cancer cells are likely to be. The chemotherapy drugs cannot penetrate large nodules of tumor tissue, which is why removing as much cancer tissue as possible is important.
CRS-HIPEC does carry risk. The mortality rate from the procedure itself has been estimated at about one to two percent in the first 30 days after surgery. Although this is not insignificant, it’s actually lower than the mortality rates for many other major gastrointestinal surgeries. Still, it’s important to be aware of the risk.
CRS-HIPEC is considered the gold standard for peritoneal mesothelioma treatment because outcomes following the procedure are significantly better than without it.
Various studies have estimated that the median survival time following this procedure is 34 to 92 months, and the five-year survival rates are between 29 and 59 percent.
The variation in outcomes is believed to be at least partly explained by differences in the amount of experience that different surgeons have with this relatively rare procedure.
Although CRS-HIPEC is considered the preferred peritoneal mesothelioma treatment, only about 50 percent of patients undergo the procedure. Some patients already have significant metastasis to lymph nodes and/or more distant organs, in which case they may not be eligible for CRS-HIPEC. Others may not be in good enough overall health to withstand such an invasive procedure.


Clinical trials are research studies of new treatment options. Some patients choose to enroll in a clinical trial in order to get early access to a novel therapy with the potential to extend life.

Palliative care focuses on quality of life rather than length of life. Some patients choose this route in order to be more comfortable during their remaining time. Palliative options may include paracentesis for draining fluid or chemotherapy for shrinking tumors that are causing symptoms.
Peritoneal mesothelioma is considered incurable, and it’s rare for patients to go into long-term complete remission from this disease. However, patients who are treated with CRS-HIPEC stand a good chance of living for several years after their diagnosis.
In order to increase the chances of a good outcome, it’s often best to be treated at a cancer center, where patients have access to specialists in medical and surgical oncology with experience in treating this rare cancer.
By submitting this form, you agree to our terms & conditions. Please read the full disclaimer