Testicular Mesothelioma
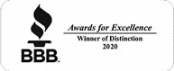
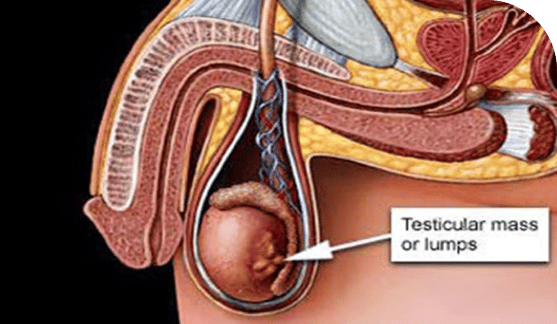
Mesothelioma is cancer that forms in the mesothelium, or membrane, that surrounds certain organs. Testicular mesothelioma accounts for less than one percent of all mesothelioma cases. It develops in the tunica vaginalis surrounding the testicles and is more common in older age groups. Studies reveal that nearly half of patients survive for at least five years after diagnosis.
Home » National Mesothelioma Law Firm » Mesothelioma Cancer » Types of Mesothelioma » Testicular Meso
Mesothelioma is a rare type of cancer that arises from the mesothelium, which is a membrane that surrounds certain organs. Testicular mesothelioma arises from the tunica vaginalis, which surrounds the testicles. This is a very rare type of cancer and is commonly misdiagnosed until after a surgical procedure.
Testicular Mesothelioma Risk Factors
Testicular mesothelioma represents fewer than one percent of all cases of mesothelioma. By contrast, pleural mesothelioma (which develops in the membrane surrounding the lung) represents 80 to 85 percent of cases, while peritoneal mesothelioma (which develops in the membrane surrounding the digestive system) represents 10 to 15 percent.
As with other types of mesothelioma, testicular mesothelioma is more common in older age groups. The median age at diagnosis is 72. This likely reflects the long latency period for mesothelioma. Pleural mesothelioma is known to take 20 to 40 years or even longer to develop, and it’s believed that testicular mesothelioma has a similar latency period in many patients. However, this cancer can occur in younger men, with up to 10 percent of patients under age 25.
Asbestos exposure is the primary known risk factor for mesothelioma in general. Pleural mesothelioma is very strongly associated with exposure to this mineral, and peritoneal mesothelioma also has an association with asbestos. There is a link between asbestos exposure and the development of testicular mesothelioma, but scientists are not yet clear on the mechanism of this link.
In pleural mesothelioma, tiny asbestos fibers in the air are inhaled and become embedded in the lung tissue. They work their way into the surrounding pleura, where they cause changes in the tissue that can lead to cancer. These fibers can also be coughed up and then swallowed, which brings them into the digestive system.
By embedding into the walls of the digestive organs and then working their way into the peritoneum, the fibers can cause peritoneal mesothelioma. However, it’s not yet understood how asbestos fibers could make their way into the tunica vaginalis in order to cause cancer in this membrane.
Testicular Mesothelioma Symptoms
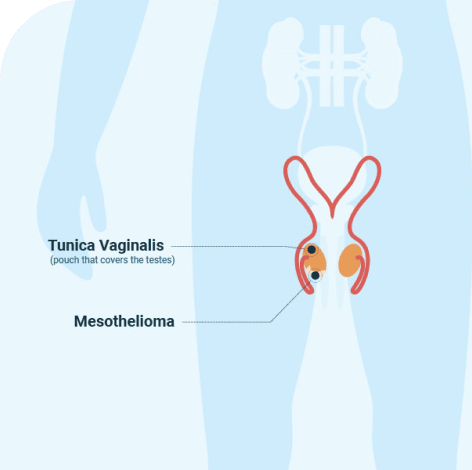
Men with testicular mesothelioma may experience a variety of symptoms, including:
- Hydrocele, which is a collection of fluid in the scrotum
- A swollen testicle
- A palpable mass in the scrotum
Similar symptoms can be caused by other conditions, many of which are more common than testicular mesothelioma. These include non-cancerous conditions like inguinal hernia, spermatocele (a cyst that develops near the testicle), varicocele (an unusual growth of veins near the testicle) and testicular torsion (a twisting of the testicle that interferes with its blood supply), as well as other types of testicular cancer. In many cases, testicular mesothelioma is initially misdiagnosed as one of these conditions.

Testicular Mesothelioma Diagnosis
After a man visits his doctor for symptoms that could indicate testicular mesothelioma, the doctor may perform a few tests in order to narrow down the diagnosis. Some tests that are commonly performed include:
Some tests that are commonly performed include:
- Ultrasound of the testicle. This can reveal the location of a fluid collection or a mass in or around the testicle.
- Blood tests can also be used. Cancers may cause a rise in particular proteins in the blood. For example, in testicular cancer, there may be higher levels of alpha-fetoprotein (AFP) and/or human chorionic gonadotropin (HCG). Doctors may test these proteins in order to look for evidence of testicular cancer. In men with testicular mesothelioma, these common proteins would not rise in the blood.
The diagnosis of any type of cancer requires a biopsy. This is a sample of tissue that is examined under a microscope by a pathologist. Based on the appearance of the cells and various tests, the doctor is able to determine whether the patient has cancer and, if so, what type.
In most cases, if a mass is discovered in one of the testicles, doctors will remove the entire testicle to examine the tissue, rather than taking just a small sample of tissue for the biopsy (as may be done for cancer in many other locations). This is the standard medical practice, because taking a sample of many types of testicular cancer can actually increase the risk that the cancer will spread. Removal of one testicle does not cause any significant health issues and doesn’t prevent a man from being fertile, so removing the whole testicle is generally recommended if any type of testicular cancer is suspected.
The most common way for testicular mesothelioma to be diagnosed is during or after surgery. One study showed that before surgery, cancer was not even suspected in 71 percent of testicular mesothelioma patients. The cancer may be discovered during surgery when doctors find a suspicious mass on the testicle. In other cases, it may not be apparent until after surgery, when a pathologist examines the tissue that was removed during the procedure and discovers mesothelioma cells in the sample.
Testicular Mesothelioma Cell Types
As with other types of mesothelioma, the histology, or cell type, of testicular mesothelioma makes a difference in the patient’s prognosis and treatment options. There are three main cell types:
- Epithelioid, in which the cells are more regularly shaped and tend to stick together in sheets or clumps. This cell type is generally the easiest to treat and has the best prognosis.
- Sarcomatoid, in which the cells have more irregular shapes and tend to spread apart from each other more easily. This cell type is generally the hardest to treat and has a poorer prognosis.
- Biphasic, which has characteristics that are intermediate between the other two cell types.
The cell type of the cancer will be determined by the pathologist when he or she examines the cancer cells under a microscope.
Testicular Mesothelioma Stages
The stage of a cancer refers to how advanced the disease is. Some types of cancer have a formal system for determining the stage based on various factors of the cancer. However, because testicular mesothelioma is so rare, a formal system has not yet been developed for determining the stage of this particular cancer.

In general, the stage of a cancer is most commonly determined using the TNM system. This system classifies three features of a cancer:
- T: the size and extent of the original tumor
- N: whether the cancer has spread to lymph nodes, either in the local area or farther away
- M: whether the cancer has undergone metastasis (spread of the cancer cells to more distant parts of the body)
These three factors are usually combined to determine a numerical stage. Stage 1 is the earliest; in this stage, the disease is still localized to the area where it first developed and has not spread. Stage 4 is the most advanced and involves spread to more distant parts of the body.
When testicular mesothelioma is diagnosed, doctors will determine the stage of the cancer before creating the treatment plan. This may involve doing one or more imaging studies, such as a CT scan, MRI and/or PET scan, to allow doctors to look for tumors in various parts of the body. Tissue that was obtained during the surgery, including the testicular tissue as well as any lymph nodes that may also have been removed, can be useful in determining the stage.
Testicular Mesothelioma Life Expectancy
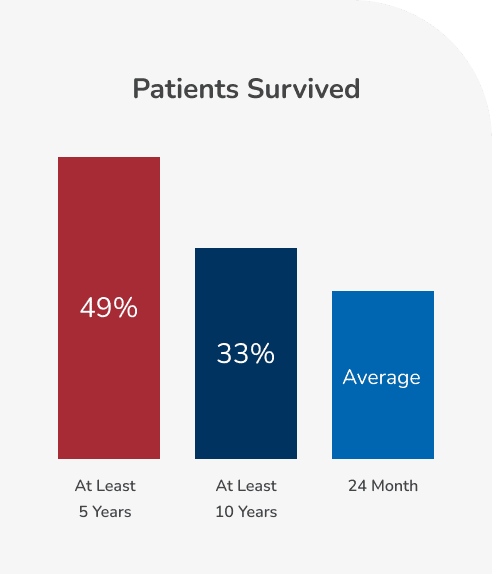
The prognosis for testicular mesothelioma patients is generally better than for those with other types of mesothelioma. One recent study showed that 49 percent of patients survived for at least five years after diagnosis, and 33 percent survived for at least 10 years. The average life expectancy is about 24 months, although this is strongly influenced by factors like the patient’s age at diagnosis (with younger patients generally living longer) and the stage of the cancer.
Patients whose disease is confined to the testicle when it’s discovered generally have a better prognosis than those whose cancer has already spread at the time of diagnosis. It’s common for testicular mesothelioma to be diagnosed in later stages, because the symptoms of the disease are so nonspecific and misdiagnosis is common.
Testicular Mesothelioma Treatment
The treatment plan for a particular patient will be determined by many factors, including the stage of the cancer, the cell type, the patient’s age and general medical condition, and patient preference. You should talk with your oncologist about the treatment plan that he or she recommends in your specific case.
The most common treatment for testicular mesothelioma is surgical removal of the cancer. Other types of treatments may be used after surgery to decrease the chances that the cancer will grow back.
For those whose cancer has already spread widely through the body before diagnosis, surgery may not be a good option. In this case, treatment may involve:
- Chemotherapy given to the whole body through an IV, usually involving a combination of two different chemotherapy drugs.
- Radiation therapy to the affected area and/or to target metastases (tumors that have grown in other areas as a result of spread of the cancer cells).
- Other palliative care options, including pain medications and physical therapy, may be used to help keep patients comfortable. Palliative care is focused on quality of life, rather than on extending life.
- Clinical trials may be an option for some patients. A clinical trial is a research study that allows patients access to a new treatment method that has the potential to extend life. Some patients with testicular mesothelioma may be eligible to participate in a study. If you’re interested in this option, you should discuss it with your oncologist, who can help you think through the risks and benefits of participating as well as help you find studies for which you may be eligible.
Treatment options include:
- Surgery, most commonly a radical orchiectomy, in which the surgeon removes the testicle on the affected side along with the spermatic cord (which connects the testicle to the rest of the body and contains the artery, vas deferens and other structures). Often, this surgery has already been performed as part of the process of diagnosis. In some cases, surgery may be needed to remove lymph nodes or other tissues where the cancer has spread. If the surgeons believe that they can remove all of the cancer through surgery, then this is often recommended.
- Chemotherapy, which is given to the whole body through an IV. This is usually adjuvant chemotherapy, which is used after surgery in order to target any cancer cells that have been left behind. Most commonly, a combination of two chemotherapy drugs is used together.
- Radiation therapy, which is sometimes also used after surgery to target remaining cancer cells.

By submitting this form, you agree to our terms & conditions. Please read full disclaimer here.